Address
304 North Cardinal St.
Dorchester Center, MA 02124
Work Hours
Monday to Friday: 7AM - 7PM
Weekend: 10AM - 5PM

,Analyzing the U.S. withdrawal from the World Health Organization, it catalyzes a fundamental restructuring of global health security architecture, with regional networks poised to fill crucial gaps in international health cooperation. This transition from centralized global governance to a more distributed, regional approach presents both opportunities and challenges for maintaining effective international health security.
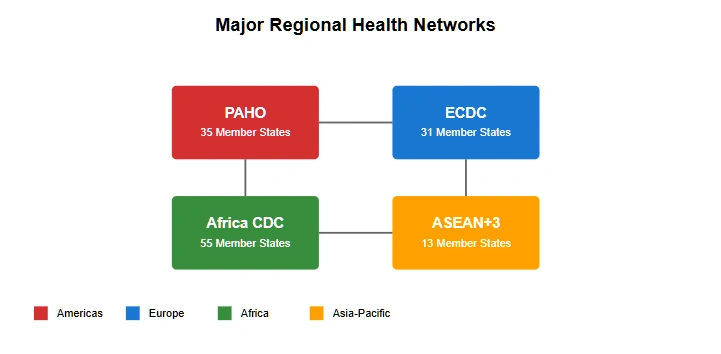
Regional health organizations, many of which predated WHO, and which the United States is planning on reinvigorating, are experiencing renewed prominence and expanded responsibilities in the wake of U.S. withdrawal. These networks, ranging from well-established institutions like the European Centre for Disease Prevention and Control (ECDC) to emerging frameworks like the Africa Centres for Disease Control and Prevention (Africa CDC), now face the challenge of coordinating health security efforts without WHO’s centralizing influence.
The Pan American Health Organization (PAHO), historically serving as both WHO’s regional office for the Americas and an independent health agency, exemplifies the complex transition ahead. As the U.S. withdrawal affects its WHO-related functions, PAHO must adapt its operations while maintaining crucial health programs across the Americas. This evolution could serve as a model for other regional organizations navigating the post-WHO landscape.
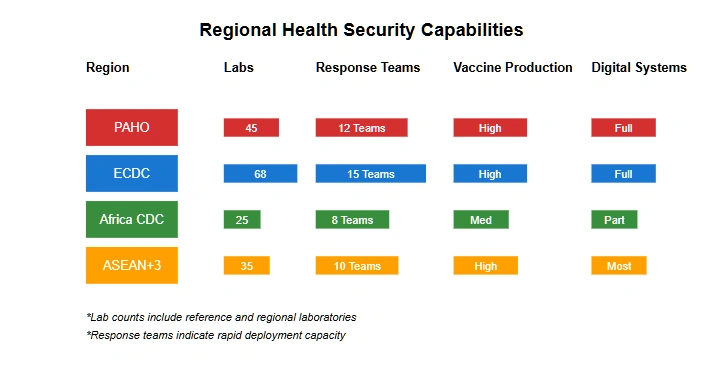
The shift toward regional frameworks necessitates new approaches to international health security coordination. Regional networks must develop enhanced capabilities in several critical areas:
Disease Surveillance: Regional organizations are expanding their disease monitoring capabilities, establishing direct connections between national health systems and regional coordination centers. This creates a more granular but potentially fragmented approach to global disease surveillance.
Emergency Response: Regional networks are developing independent rapid response capabilities, including stockpiles of medical supplies and deployable medical teams. These efforts aim to provide more immediate and contextually appropriate responses to health emergencies.
Research Coordination: The development of regional research networks and data-sharing platforms aims to maintain scientific collaboration while accommodating varying regulatory frameworks and research standards across regions.
The Pan American Health Organization’s adaptation to the post-WHO environment provides crucial insights into the challenges and opportunities facing regional health networks. PAHO’s unique historical position as both a WHO regional office and an independent organization offers valuable lessons for other regions developing autonomous health security capabilities.
Europe’s response to the changing global health landscape builds upon the established capabilities of the European Centre for Disease Prevention and Control (ECDC) while developing new mechanisms for international cooperation. The European Health Union initiative, accelerated by the U.S. withdrawal from WHO, represents an ambitious attempt to create a comprehensive regional health security framework.
Key elements of the European approach include:
The European Health Emergency Preparedness and Response Authority (HERA) has expanded its mandate to fill gaps left by reduced WHO coordination. This includes enhanced powers for emergency procurement, stockpile management, and cross-border health threat response.
Enhanced surveillance networks now connect national health systems more directly, creating a more robust early warning system for the region. The European Health Data Space initiative facilitates secure sharing of health data while maintaining strict privacy standards.
Cross-border healthcare cooperation has intensified, with new protocols for patient transfer, medical resource sharing, and coordinated emergency response. These mechanisms proved crucial during the COVID-19 pandemic and continue to evolve.
The Africa Centres for Disease Control and Prevention (Africa CDC) has emerged as a central player in coordinating health security across the continent. Building on experience gained during previous health emergencies, including Ebola outbreaks and the COVID-19 pandemic, Africa CDC has developed increasingly sophisticated capabilities for regional health coordination.
The organization’s New Public Health Order initiative represents a comprehensive approach to building regional health security capacity. This includes:
Development of the African Pandemic Preparedness Fund, which provides dedicated resources for emergency response without relying on external funding sources.
Establishment of Regional Collaborating Centers across the continent, creating a distributed network for disease surveillance and response coordination.
Implementation of the African Vaccine Manufacturing Initiative, aimed at reducing dependency on external suppliers for essential vaccines and medications.
The Asia-Pacific region presents unique challenges for regional health security coordination, given its diverse political systems, varying economic development levels, and complex geopolitical dynamics. Moreover, China’s attempts at health diplomacy in the wake of the COVID-19 Pandemic produce a context in which it may attempt to replace the United States as the WHO’s informal leader. Multiple overlapping frameworks have emerged to address these challenges:
The ASEAN Center for Public Health Emergencies and Emerging Diseases has expanded its role, providing crucial coordination for Southeast Asian nations. Its digital disease surveillance platform has become a model for regional early warning systems.
The Asia-Pacific Economic Cooperation (APEC) Health Working Group has developed new mechanisms for sharing health intelligence and coordinating emergency response among member economies. This includes protocols for maintaining essential supply chains during health crises.
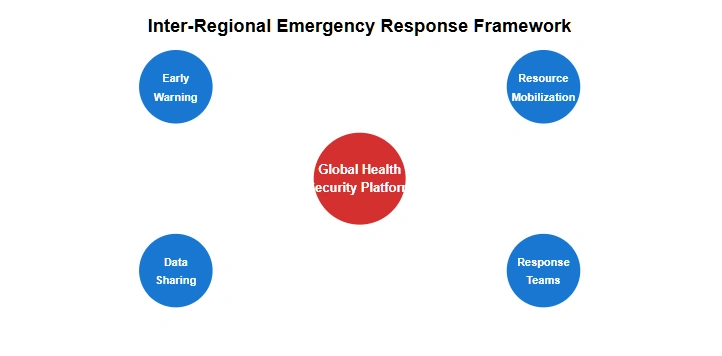
The fragmentation of global health governance has necessitated new approaches to coordination between regional networks. Without WHO’s centralizing function, regional organizations have developed bilateral and multilateral arrangements to maintain essential international health cooperation.
The Global Health Security Coordination Platform (GHSCP), a new initiative involving major regional health organizations, attempts to provide structure for inter-regional cooperation. This platform facilitates regular communication between regional centers, standardizes data sharing protocols, and coordinates emergency response capabilities across regions.
Key elements of inter-regional cooperation include:
Cross-Regional Disease Surveillance: Regional networks have established direct connections between their surveillance systems, creating redundant monitoring capabilities that help compensate for the loss of WHO’s global surveillance network. These connections enable rapid sharing of information about emerging health threats across regional boundaries.
Emergency Resource Sharing: Formal agreements between regional organizations enable rapid mobilization and sharing of medical resources during crises. These arrangements include protocols for sharing vaccine supplies, deploying medical personnel, and coordinating logistics support across regions.
Research and Data Exchange: Inter-regional research networks maintain scientific collaboration across geographic boundaries. Standardized data sharing agreements and common research protocols facilitate continued international cooperation in medical research and development.
The transition to a regionally-focused health security architecture presents significant challenges that must be addressed for the system to function effectively:
Standardization and Compatibility: Different regional networks employ varying technical standards, reporting protocols, and operational procedures. Harmonizing these differences without a central coordinating body requires extensive bilateral and multilateral negotiations.
Resource Disparities: Regional networks operate with vastly different resource levels, creating potential gaps in global health security coverage. Wealthier regions must balance domestic priorities with the need to support developing regions’ health security capabilities.
Political Complications: Regional health cooperation often intersects with complex political relationships and competing strategic interests. Managing these tensions while maintaining effective health security cooperation requires careful diplomatic navigation.
The evolution of regional health networks signals a fundamental shift in how the international community approaches health security challenges. Several key trends will likely shape the future development of this new architecture:
Technological Integration: Advanced digital platforms and artificial intelligence systems are enabling more sophisticated coordination between regional networks. These technologies could help overcome some of the challenges posed by the fragmentation of global health governance.
Capacity Building: Regional organizations are investing heavily in developing independent capabilities that were previously provided by WHO. This includes building laboratory networks, training programs, and emergency response systems tailored to regional needs.
Flexible Partnerships: The emerging system emphasizes adaptable cooperation frameworks that can respond to changing health security challenges. This includes both formal agreements between regional organizations and informal coordination mechanisms that facilitate rapid response to emergencies.
The shift toward regional health security networks represents both a challenge and an opportunity for the international community. While the loss of WHO’s centralizing function creates certain risks, the emergence of more robust regional capabilities could ultimately strengthen global health security by creating more resilient and adaptable response mechanisms.
Success in this new framework requires sustained commitment to international cooperation, even as it takes new forms. Regional networks must balance their independence with the need for effective cross-regional coordination. The development of new technologies and coordination mechanisms offers promising tools for maintaining global health security in an increasingly regionalized landscape.
The future effectiveness of this evolving system will depend largely on the ability of regional networks to strengthen their individual capabilities while maintaining robust inter-regional cooperation. As this new architecture continues to develop, the international community must remain focused on the ultimate goal: protecting global health security through effective coordination and cooperation, regardless of the specific organizational frameworks involved.
This transition period offers a crucial opportunity to build more resilient and responsive health security systems. While challenges remain, the emergence of strong regional networks, supported by sophisticated coordination mechanisms and technological tools, provides a foundation for maintaining and potentially enhancing global health security in the post-WHO era.
[…] CBSA (border services), CSE (communications security, for cyber protection), Health Canada (for health security like pandemic measures or medical readiness), Transport Canada, etc. This mirrors the model from […]
[…] The country’s health diplomacy rests on several pillars: bilateral health agreements, multilat…, medical team deployments, infrastructure development, and pharmaceutical exports. This comprehensive approach has already yielded significant influence, particularly in Africa and Southeast Asia, where Chinese medical teams and health infrastructure projects have established long-term relationships with local health systems. […]
[…] As the United States steps back from WHO participation, regional health security networks may take o… The Americas region, in particular, faces both opportunities and challenges in adapting to this new reality. The existing infrastructure of the Pan American Health Organization (PAHO) could provide a foundation for enhanced regional cooperation, though the U.S. withdrawal from WHO may complicate these relationships given PAHO’s status as a WHO regional office. […]